COOPERATION MODEL
ARTIFICIAL INTELLIGENCE
PRODUCT ENGINEERING
DevOps & Cloud
LOW-CODE/NO-CODE DEVELOPMENT
INDUSTRY
FRONTEND DEVELOPMENT
CLOUD DEVELOPMENT
MOBILE APP DEVELOPMENT
LOW CODE/ NO CODE DEVELOPMENT
EMERGING TECHNOLOGIES








AI is starting to show up in nursing, but it is still at an early stage. Only 4.5% of nursing facilities leverage AI in 2025. Use is somewhat higher in outpatient clinics (OPD) and ambulatory care, but even there, it is limited and uneven.
Where AI is in use, it is in a few practical areas. Documentation, basic triage support, patient monitoring, and some day-to-day routine tasks. Most of this adoption is happening at the individual clinics, home-health agencies, and small providers. Organization-wide rollouts are still uncommon.
Nurses themselves are generally open to AI. Many see potential value, especially when it reduces paperwork. At the same time, there are concerns about data privacy. In this article, we look at where AI stands in nursing today and the challenges around its use.
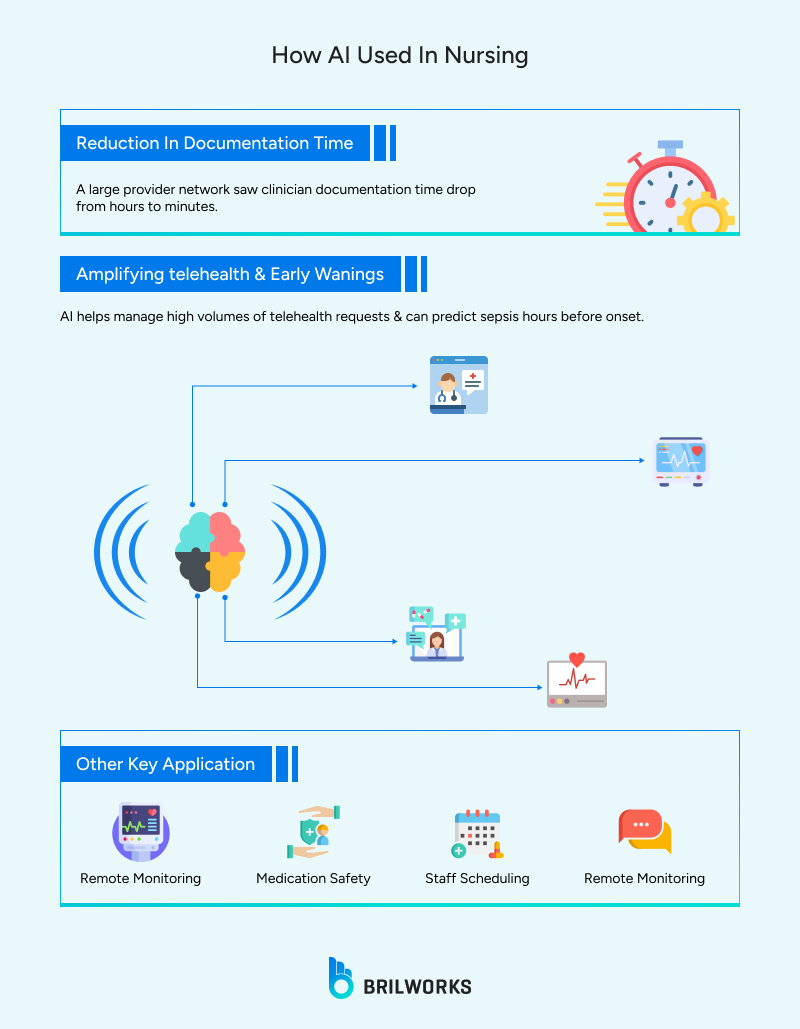
Documentation is the most common application of AI today, across multiple industries, including healthcare. AI tools are efficient enough to record conversations round-the-clock and turn them into draft notes or summaries.
Ochsner Health, a large provider network, has been using DeepScribe across its 4,700 clinicians, and the observed documentation time dropped by about 75%, from hours to minutes per note.
In practice, notes created by AI tools are treated as finished. They need to be reviewed and corrected. These tools may not provide accurate details. Accents, interruptions, and clinical nuance can be problems. But the main benefit is saving time on routine documentation.
Telehealth usage increased 38X from the pre-COVID period. AI has amplified it further. Nurse-led telehealth services increasingly turn to leverage AI to handle mass requests. These tools can walk through patient information and help identify cases.
They are effective, too. There are thousands of case studies surfacing online, citing that the implementation of AI tools in healthcare helps improve service delivery. A San Francisco researcher used AI in nursing care to predict sepsis 12 hours before onset.
In hospitals, early warning scores are now also used to prioritise patients who may be at risk of getting worse. Trust is still a challenge because these tools may not explain why a case is flagged.
Digitalisation gave healthcare professionals a way to connect with patients and doctors without visiting in person, whether for consultations or booking appointments. But data management remained a big issue, not only in healthcare but across every industry.
The speed at which AI works with large volumes of data is starting to address this problem. Remote patient monitoring(RPM), when combined with AI capabilities, can capture more information than humans can handle alone and turn it into meaningful inputs for decision-making. However, human involvement is still required. Without it, the output may remain raw or incomplete.
Remote patient monitoring grew rapidly during COVID-19, and since then, it has continued to grow steadily.
Newer systems can analyse data to detect patterns and trigger alerts.
Early warning alerts are more efficient.

An AI-aided web assistant used at a hospital training center in Ankara was reviewed for medication checks and flagged about 90% of risky drug–drug interactions and inappropriate medications.
Nursing homes and small hospitals are progressively using AI tools to help with medication checks. These tools can flag drug interactions. This technology is currently being treated as an assistant, which can provide astonishing results if provided with accurate data. Healthcare professionals treat this as an added safety layer, not a replacement for their own judgment.
The use of AI in staffing, scheduling, and day-to-day tasks is gradually becoming more common. For example, AI tools are now used to schedule appointments and check availability, whether on the doctor’s side or the patient’s side. Among AI-using hospitals, billing/scheduling AI is common. These tools look at how many appointments are already booked and identify open time slots where more appointments can be added.
Healthcare apps(chatbots), when they have access to the right information, can answer common patient questions without involving clinical staff. In addition, agent-based AI systems can update manual records, spreadsheets, CRMs, and EHRs as part of routine administrative work.
By offloading entry-level and repetitive tasks, healthcare teams are noticing improvements with healthcare apps, especially for clinicians who spend less time on administrative work.
But adoption here is limited. Many small providers still use legacy systems, and without modernising, running or integrating AI is complex. Cost is another barrier, and for many teams, the benefit is still not clear enough to justify the effort of implementation.
AI chatbots come in different forms. Take an example; an e-commerce platform can use them alongside a customer service team, and healthcare organizations use them in a similar way. They are mainly used to handle basic queries, while keeping humans in the loop for more complex issues. When used this way, they can improve customer service. Chatbots not only function as CX tools internally but also can be leveraged to train staff.
New nurses ask basic questions like "How do I log vitals in our EHR?" or "What’s the protocol for fever checks?" The bot pulls answers from policy docs.
There are so many practical use cases of AI in nursing.
Overall, AI use in healthcare is modest. Nursing homes and residential care facilities, in particular, show slow uptake. Older systems and unclear rules all contribute to this gap.
At the same time, awareness is much higher than actual use. Many nurses know about AI tools and want support that reduces paperwork and mental load. Interest is there, but full deployment is not yet common.
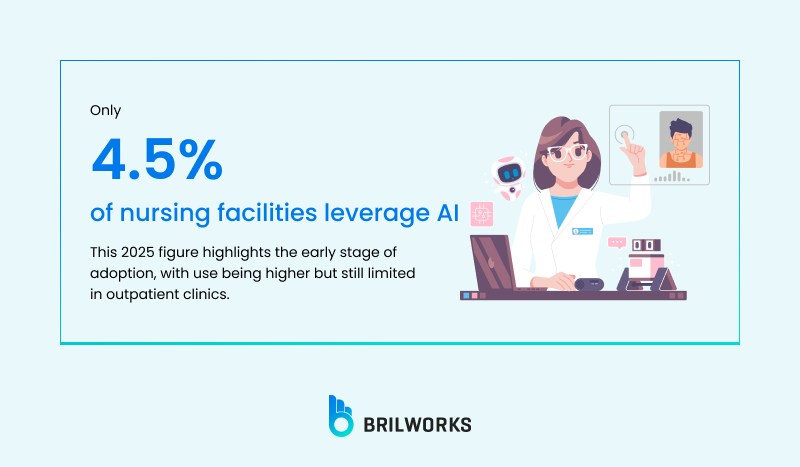
Overall, AI use in healthcare is about 8.3% in US healthcare organizations in 2025, up from 5.9% in 2023.
71% hospitals use predictive AI in EHRs, but nursing-specific tools trail.
55% cite privacy and skills issues as blocks.
Legacy EHRs (60% barrier), regulations, and training gaps hold back uptake.

In short, full rollout is rare in SMEs. For most small and mid-size providers, the barriers are practical. Privacy is a major concern; regulatory rules are not clear and are otherwise complex. Without deep integration within the healthcare systems, the AI advantage is very limited.
AI use in nursing today is uneven and evolving. Most adoption is happening around specific problems such as documentation, monitoring, and scheduling, rather than across entire systems. Where tools reduce everyday friction. The pattern of AI adoption in nursing is consistent: progress is little.
For owners interested in implementation, it begins with a clear understanding of workflow, limitations of AI, regulatory nuances, and so on. Healthcare development and consultants can help you at this stage if you want to build a strong, scalable foundation.
Get In Touch
Contact us for your software development requirements
Get In Touch
Contact us for your software development requirements