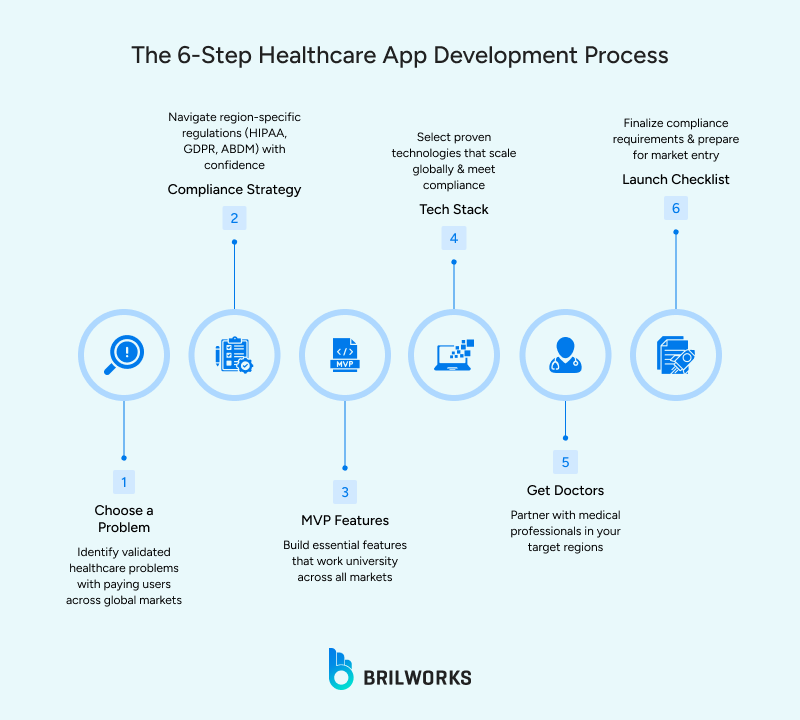
Phase 1: Conceptualization and Strategy
1. Define a Specific, Measurable Problem
Every strong healthcare app starts with a clear, measurable medical or operational problem that costs time, money, or health today. The easier the pain is to measure, the more meaningful the solution.

For example:
- Hospitals lose significant revenue from patient no-shows and cancellations
- Nurses spend hours weekly on manual documentation instead of patient care
Studies also show remote cardiac monitoring helps prevent readmissions within the first 30 days after discharge. Insights like these connect your idea to real clinical value, not assumptions.
2. Choose One Primary User Group
Once the problem is defined, you do not jump into feature ideas. You first identify who will use the solution directly. Their needs shape everything.
Patients, clinicians, and admins see the same workflow from different angles. A doctor wants less charting. A patient wants easy tracking. An administrator wants reduced operational waste. You cannot serve all perfectly on day one. You choose one and succeed there first.
3. Confirm Compliance From Day 1
Before any wireframe exists, you check which
regulations your product must follow. If the app collects or touches Protected Health Information (PHI), HIPAA (Health Insurance Portability and Accountability Act) applies in the US, and GDPR (General Data Protection Regulation) applies in Europe.
If the app influences diagnosis or treatment, it may be classified as Software as a Medical Device, which means you may need approval from authorities such as the FDA (U.S. Food and Drug Administration) or CE (Conformité Européenne) marking in Europe.
Compliance rules are not boring legal text.
They define architecture, hosting methods, and how data flows. Teams who delay this end up rebuilding core systems later, wasting months.
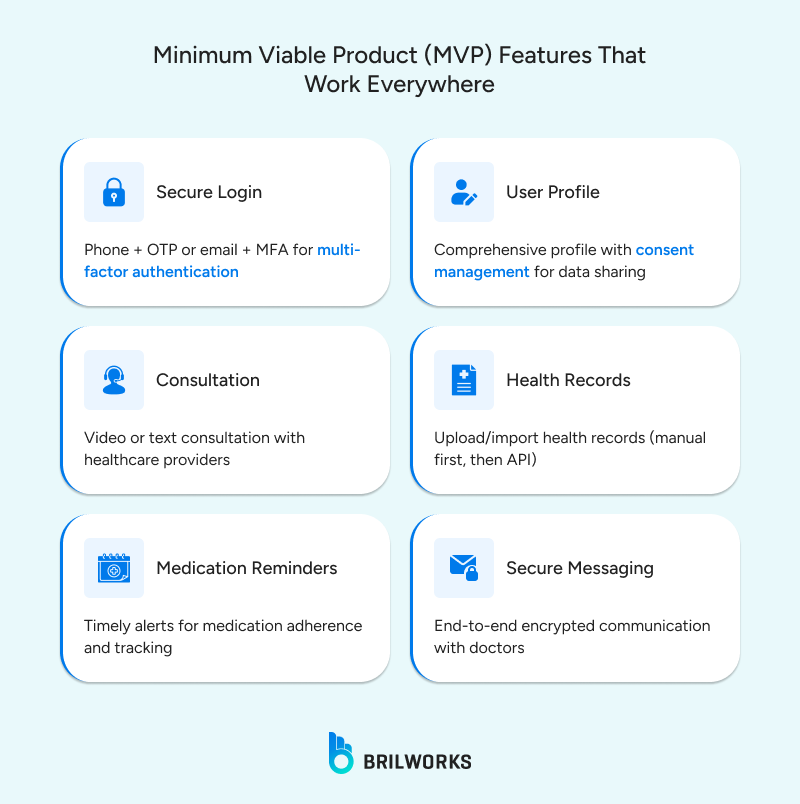
4. Design the First Real Workflow (MVP)
With problem, user, and compliance aligned, you plan the first workflow that must always work in the real world. Healthcare
MVPs are not feature collections. They are one strong workflow proven valuable.
A healthcare MVP succeeds when it solves one job well, consistently, in clinical or patient environments. Not when it has ten half-working modules.
Phase 2: Design and Architecture
1. UX Built for Real Clinical Pressure
A healthcare app is used by people who are stressed, rushed, or dealing with discomfort. The design must remove thinking. A clinician should not spend five seconds trying to find a key function while a patient waits. A patient managing symptoms should not decode icons when they are already anxious. The best healthcare UI feels obvious in the first second: clear actions, fast access, and text legible for all ages.
One quick rule: If a first-time user cannot complete the core task without guidance, fix the design.
2. Onboarding Must Build Trust and Confidence
Connecting to wearables, verifying medical identity, or syncing records can confuse users if not guided step by step. People abandon apps when clarity breaks or instructions feel intimidating. Smooth onboarding keeps both clinicians and patients willing to continue.
3. Security Is a Core Design Decision
Security cannot be patched later. Healthcare data includes identity, history, billing info, everything fraudsters target. This is why:
- Data must be encrypted everywhere
- Access permissions must match job role
Audit logs need to track who viewed what and when. Hospitals will only approve technology where security is provable, not promised.
4. Integration Makes You Part of Real Care
Your app does not replace hospital systems, it joins them. Electronic Health Record (EHR) interoperability is what moves your product from “app store tool” to “clinical tool.” That requires
HL7 (Health Level Seven, a set of international health data standards) for legacy systems or FHIR (Fast Healthcare Interoperability Resources, a newer interoperability standard) for modern ones. Without secure integration, your app becomes isolated and soon forgotten in a real healthcare workflow.
Phase 3: Development, Testing, and Deployment
The difference between “it works” and “it works in healthcare”
1. Build for Compliance and Integration First
When development begins, your tech choices should support compliance and interoperability. Not what is trending. Native iOS and Android are strong choices for apps that require precise access to sensors or advanced accessibility features.
Cross-platform tools like React Native or Flutter help when time to market is important and hardware access is simpler. On the backend, Node.js or Python remains reliable because both offer strong API security and support healthcare data formats.
One non-negotiable rule: Your hosting partner must sign a Business Associate Agreement (BAA, a legal contract ensuring appropriate protection of health information)
Without a
BAA, storing PHI is simply not allowed. The entire cloud strategy collapses there.

2. Validate in Real Clinical Environments
Normal QA testing checks functionality. Healthcare
testing checks survival in real use. That means observing how people interact when they are busy, tired, or under pressure. A doctor moving through patient rounds, a nurse jumping between tasks, or a patient checking symptoms late at night.
Every hesitation exposes a design flaw. Friction you do not see in a lab becomes a real barrier in a clinic. Usability is successful only when real users complete tasks confidently the first time.
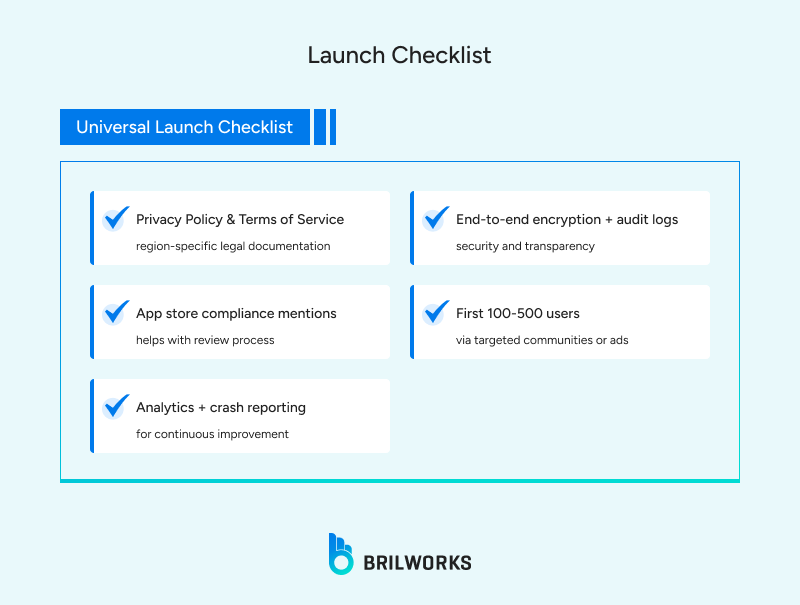
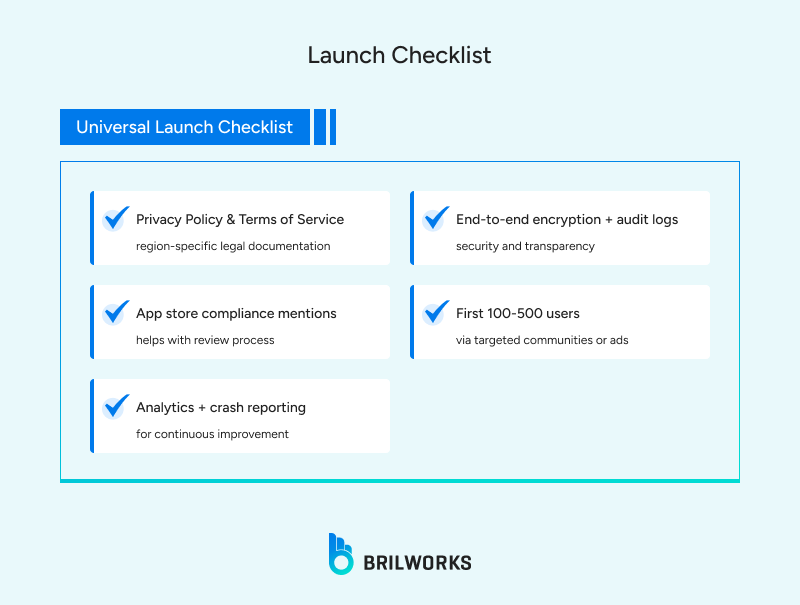
3. Prove Compliance Before You Ship
Before launch, compliance teams must review how health data is handled. Penetration tests should confirm no vulnerabilities remain. App stores now require health apps to clearly explain data usage and protection. You must be able to show exactly how PHI flows through the system and who controls access.
Hospitals will only approve a product they can defend legally and operationally.
4. Ownership After Launch Is Continuous
Healthcare technology never “finishes.” Regulations evolve.
Security threats increase. Workflows change. You update because reliability is a responsibility. Feedback from clinicians and patients shapes improvements.
And
performance monitoring becomes part of everyday operations because failure at the wrong moment is not acceptable in care settings.
A healthcare launch is not the finish line. It is the moment accountability begins.
Best Practices
There are certain habits that consistently separate healthcare apps that get adopted in real clinical settings from those that are ignored after a week.
- Unclear messages force users to guess. A simple explanation with a way to recover keeps workflows moving under pressure.
- Large text, high-contrast colors, screen reader support and clear navigation make your product usable for patients with low comfort or visual limits.
- Slow loading or lag kills attention. Real care settings cannot tolerate delays while people are waiting for action.
- Data at rest and data in transit must always stay protected. Without it, the product never reaches hospitals.
- Audit logs help IT teams trust your product. It also supports investigations if anything goes wrong later.
- Connecting devices or authorizing identity must feel guided. Friction here destroys early adoption rates.
- Measurements, history and alerts must be reliable. Wrong data is worse than no data in healthcare.
- If your product cannot talk to existing systems, clinicians will stop using it because it adds work instead of reducing it.
- Doctors, nurses and patients do not need the same data. Limit access based on role to keep both security and clarity intact.
- Healthcare apps do not get a free pass. Outages or bugs hit real patients. Ongoing support is part of the product responsibility.
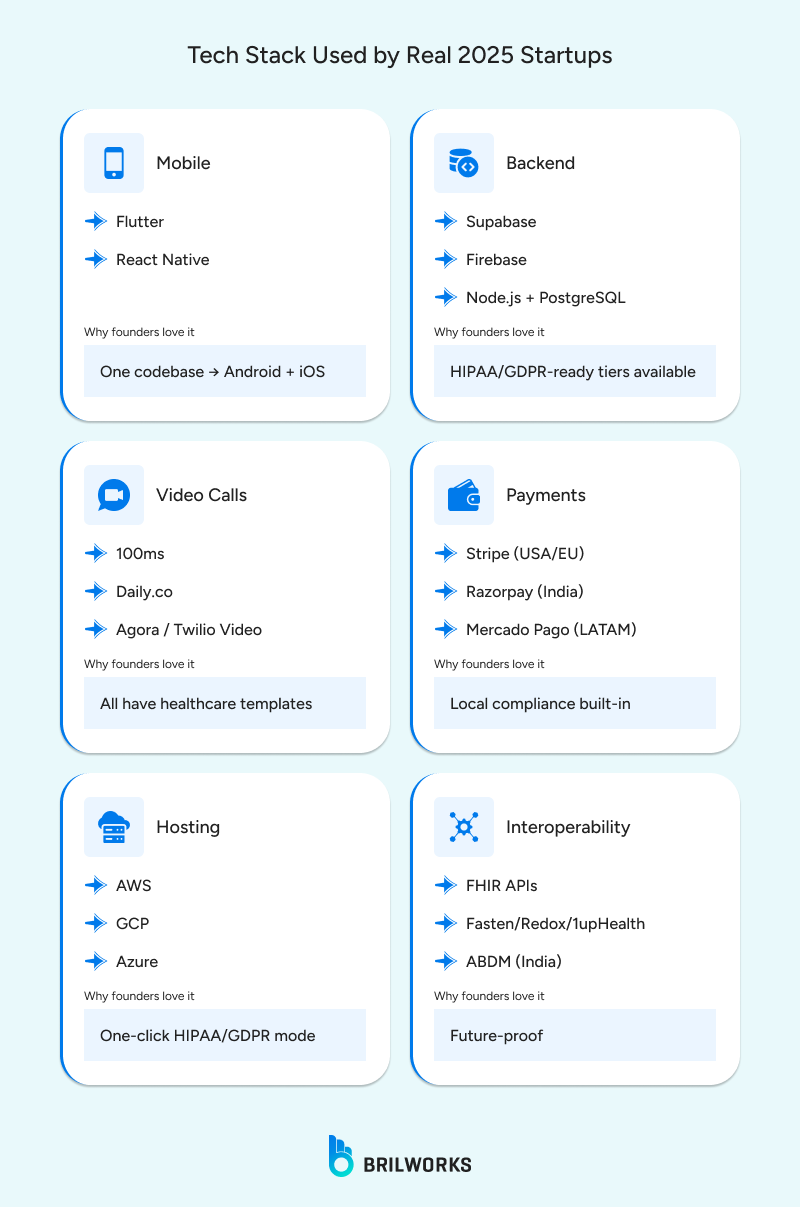
Technology Stack for Healthcare Development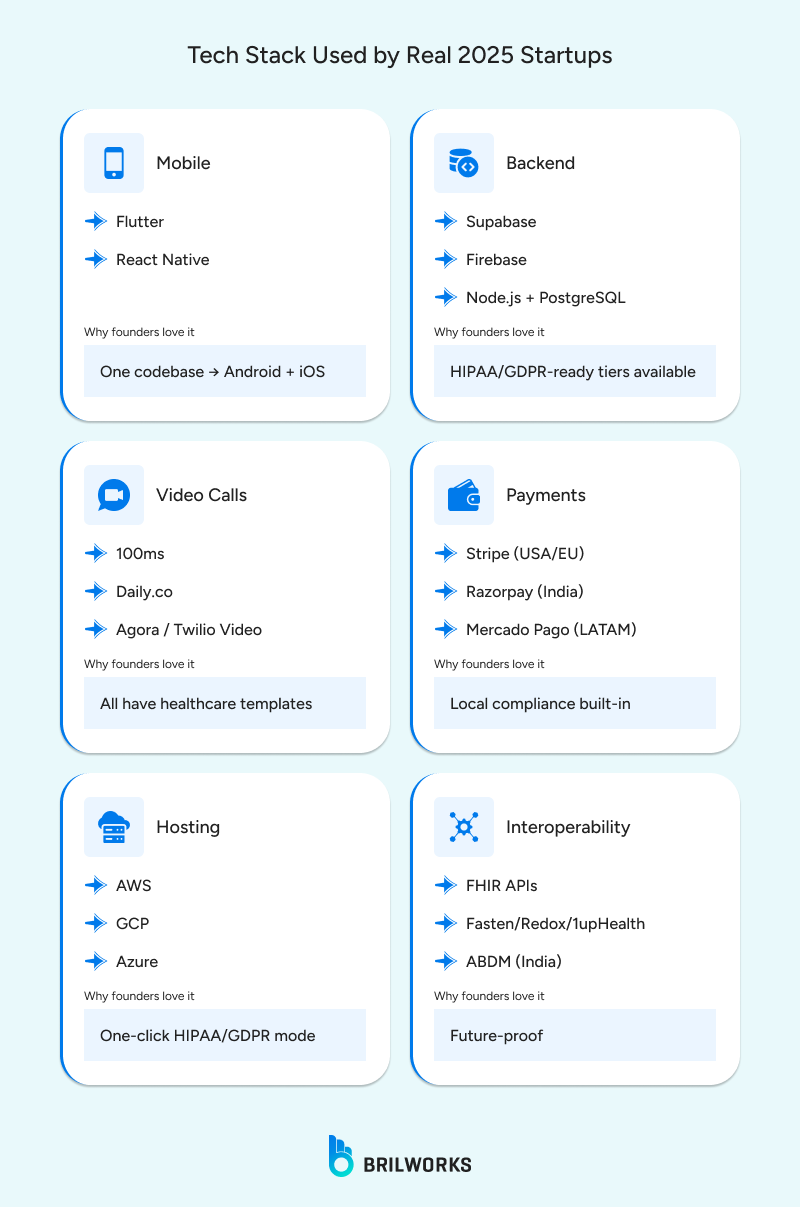
1. Frontend (Mobile App Layer)
Patient-facing apps often prioritize faster releases, device compatibility, and smooth UI. That is where
React Native or Flutter gives a strong advantage. They offer a single codebase, faster updates, and enough access to wearables through secure SDKs.
But when the product demands more accurate hardware-level access building natively in Swift (iOS) or Kotlin (Android) delivers better reliability.
2. Backend, Database, and Cloud
Healthcare backends are typically
Node.js or Python because they provide strong validation, secure authentication flows, and connectors for standards like FHIR (Fast Healthcare Interoperability Resources, a healthcare data format) and HL7 (Health Level Seven, older data-sharing standards).
For storing PHI (Protected Health Information), PostgreSQL is widely used because it is stable and handles structured clinical data well. Hosting must be inside a HIPAA (Health Insurance Portability and Accountability Act, U.S. health data law)/GDPR (General Data Protection Regulation, E.U. data law)-compliant environment, like AWS (Amazon Web Services) or Azure (Microsoft's cloud service), with a formal Business Associate Agreement (BAA). If the cloud cannot legally store medical data, nothing moves forward.
Quick Comparison
| Layer | Fast Delivery | High Precision |
| Mobile App | React Native / Flutter | Swift / Kotlin |
| Backend | Node.js | Python |
| Database | MongoDB | PostgreSQL |
| Hosting | Any cloud with BAA | AWS / Azure Healthcare |
| Interoperability | FHIR APIs | FHIR + HL7 |
How to Choose the Right Healthcare Tech Stack
- Pick mobile technology based on hardware dependency
- If your app depends on precise medical sensors, native development is safer. If your focus is speed and broad accessibility, React Native or Flutter help you ship updates faster.
- Choose backend frameworks that make compliance easier
- Node.js and Python both allow secure API (Application Programming Interface) development and strict validation rules. They offer better support for FHIR (Fast Healthcare Interoperability Resources)/HL7 (Health Level Seven) libraries so your product can communicate with hospital systems.
- Use a database designed for accuracy and auditability
- PostgreSQL supports strong data integrity and transactional operations — critical when storing measurements, prescriptions, history, or anything that must never be corrupted.
- Deploy on healthcare-approved cloud platforms only
- Your provider must sign a Business Associate Agreement (BAA, a legal contract ensuring health data protection). Without it, storing PHI (Protected Health Information) becomes illegal, and the entire infrastructure fails compliance audits.
- Plan integration early to avoid becoming a standalone tool
- Interoperability decisions should be part of early architecture. Hospitals won’t adopt products that cannot sync data to their existing systems.
Final Thought
Healthcare apps succeed when they solve one real clinical or patient problem and respect the rules that protect people. The products that thrive in hospitals do not win because of flashy UI or the latest framework trend. They win because they reduce friction in care, earn trust from compliance teams, integrate with existing workflows, and keep improving as the needs of patients and clinicians evolve.
Everything shared in this guide reflects how real healthcare engineering works. There are no shortcuts in interoperability. There is no ignoring compliance and hoping later goes smoothly. Security is not a feature that gets added after launch. If the product influences care, then reliability becomes a clinical requirement.
If you are planning to build a healthcare solution, you now understand the level of clarity and responsibility it requires. Whether your focus is remote monitoring, telehealth, medication tracking, or EHR connectivity, you need a team that knows how to navigate regulations, build secure foundations, and support long-term performance in actual clinical environments.
Healthcare software is not just another digital product.It becomes part of how someone is treated. That is the responsibility. That is also the reward.