COOPERATION MODEL
ARTIFICIAL INTELLIGENCE
PRODUCT ENGINEERING
DevOps & Cloud
LOW-CODE/NO-CODE DEVELOPMENT
INDUSTRY
FRONTEND DEVELOPMENT
CLOUD DEVELOPMENT
MOBILE APP DEVELOPMENT
LOW CODE/ NO CODE DEVELOPMENT
EMERGING TECHNOLOGIES







In 2021, Ireland’s Health Service Executive (HSE) fell victim to a Conti ransomware attack. It began with a phishing email that exploited a known vulnerability in Microsoft Exchange Server. According to The Guardian, the fallout was immediate; IT systems across 54 hospitals went down.
It may have been the first time an entire national healthcare system was taken offline by ransomware. Staff had to return to pen and paper. Outdated software, some machines were still running Windows XP, making recovery slower and more difficult. Modernization is not only a desirable option, but it also safeguards against potential threats that can arise from outdated systems.
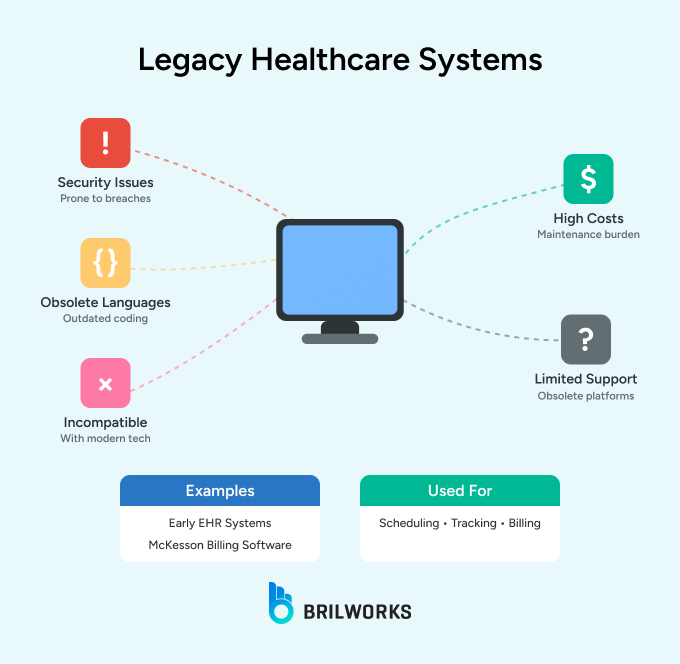
Legacy software or systems in healthcare refer to outdated software or hardware that doesn’t support modern requirements. They may be developed using old programming languages and technologies. Even though they are prone to security vulnerabilities, these software or services continue to be used due to high replacement costs and are deeply integrated into critical processes.
In healthcare, traditional Electronic Health Record (EHR) systems are examples of legacy systems. They are typically used for scheduling, patient tracking, resource allocation, or even as billing platforms, such as McKesson’s older billing software.
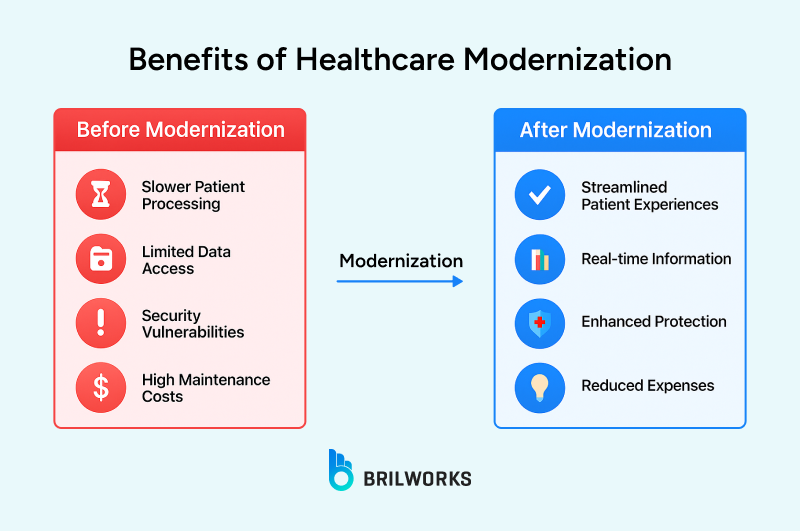
One of the main reasons companies modernize legacy systems is to improve security. In many cases, these systems are expensive to maintain. And because they’re so deeply embedded in the business, replacing them isn’t an easy decision for business owners.
However, legacy systems have a direct impact on security, cost, and the ability to innovate.
According to Gartner, 40 to 80% of the IT budget often goes into maintaining them. Experts also point out that inefficiencies and the growing difficulty of finding specialized talent to maintain these systems are driving up costs.
In healthcare, especially, maintaining data security and compliance is essential. Modernization helps boost operational efficiency and productivity.
Most businesses link their security gaps to these legacy systems. At the same time, it’s not easy to make them work with modern technologies. And as we mentioned earlier, maintaining them can often be more expensive than adopting new solutions. Let’s take a look at some of the key challenges involved.
Outdated encryption protocols like SSL are no longer considered secure by modern standards. Systems that still rely on them can be potentially vulnerable to cyberattacks. On top of that, maintaining less secure platforms can be more expensive.
When security protocols are outdated, it also becomes more challenging to meet compliance requirements, such as HIPAA or other regulations. This creates roadblocks for innovation and slows down progress.
Connecting legacy systems with newer cloud technologies and frameworks isn’t straightforward. Many older EHRs, for example, don’t support modern standards like HL7 FHIR. Because of that, their ability to work smoothly with cloud platforms or IoT-based medical devices is limited. It creates friction where there should be flexibility.
Systems running on outdated technologies like COBOL are hard to maintain today, mainly because there are fewer professionals who still work with them. Hiring those specialists often costs more than hiring engineers for modern tech stacks.
“Most of the clients we've worked with on modernization projects came in mainly because of rising maintenance costs of legacy infrastructure,” said the CTO at Brilworks.
Legacy systems often have slow processing speeds and limited scalability, and do not support many concurrent users. To consider an example, an old hospital management system may take several minutes to get and process a patient's history.
Experts agree that many modernization projects don’t happen simply because business owners feel it’s easier to keep running what already works. And they’re not entirely wrong.
Sometimes, it turns out to be more expensive than sticking with the current system. That’s why it’s important for decision-makers to understand when it actually makes sense to modernize. Let’s look at when modernization might not be the right move and when it is.
Modernization can mean anything from minimal updates to doing a complete infrastructure overhaul. There’s no single way to do it; there are several approaches. We’ll quickly go over some of the popular approaches to give you a clear idea of how modernization can look in different situations.
Encapsulation is wrapping legacy systems with modern interfaces without altering the core system. For example, a hospital might use an API layer to connect an old EHR to a new patient portal. This approach is cost-effective but limited by the underlying system’s constraints.
Rehosting, or "lift and shift," is moving legacy systems, without changing or redeveloping the code, to a modern infrastructure (e.g., cloud).
Rehosting is best when an organization needs immediate scalability without needing to redevelop everything from scratch or figure out its code entanglement. For example, moving the billing system to AWS boosts uptime and helps save on onboarding hardware costs.
Refactoring is when you change the structure of the existing code base to improve performance without changing functionality. Refactoring is appropriate when an application has good core functionality but is underperforming.
For example, refactoring a legacy EHR to modern APIs to improve interoperability.
Rearchitecting changes the architecture of the system, often by way of microservices or API-first designs. This is appropriate for healthcare systems that need to be scalable and also be interoperable. For example, rearchitecting a billing system into microservices allows more integration with a variety of insurance platforms.
Replacement includes commercial off-the-shelf (COTS) approaches or systems developed from scratch. This option is best suited for systems that are entirely obsolete. For example, replacing an old EHR with Epic or Cerner will ensure functionality and compliance in a modern manner.
Rebuilding is defined as redeveloping the system "from the ground up." It is used when you have no other options. An example of this might be a hospital rebuilding a custom clinical decision support system because it wants to include AI analytics within the software application.
When running a healthcare organization with legacy or legacy-integrated systems, it is critical to take a structured approach to the modernization process to reduce downtime and create a successful path toward modernization.
Identify all of your legacy systems; document dependencies, workflows, and pain points. Define your modernization objectives to ensure they align with the organization's higher priorities (e.g., improving patient outcomes or reducing costs).
Work with your clinical staff, IT team, administrative staff, and patients to elicit requirements; for example, while clinicians may want to see real-time data, administrators may push for cost savings.
Understanding where legacy data will go and migrating that data to the new or modernized system in a clean and validated way is key. For example, FHIR compliance mapping for patient records is important for ensuring interoperability. Ensure you maintain data integrity through proper testing and validation.
Take an incremental approach to your implementation and deployment schedules to avoid disruption. For example, deploy the new patient portal before you replace the entire EHR. The implementation schedule should reflect goals, priorities, and what is likely to have the best impact.
Plan to incorporate Alpha, Beta, and User Acceptance testing and validation in your project plan. Involve your clinical staff in user acceptance testing to demonstrate that the new system meets their actual needs.
Go live at the best time for your organization, i.e., during your slowest volume times. Full personnel training of the new system is critical to reducing subsequent frustration with end-users. Consider running systems in parallel for some time after going live. Measure success by metrics such as uptime, adoption, and patient satisfaction after going live and for the foreseeable future.
Interoperability and compliance are essential components of healthcare IT modernization. The key interoperability standards, as well as the compliance requirements, include the following:
Therefore, any modernization effort must incorporate these standards to facilitate interoperability and to comply with regulations.
|
Deployment Model |
Best For |
Security Considerations |
|
Public Cloud |
Non-sensitive workloads |
Requires robust encryption |
|
Private Cloud |
Protected health information |
Enhanced control and compliance |
|
Hybrid Cloud |
Mixed workload environments |
Segmentation of sensitive data |
AI and cloud computing are game-changers for modernizing healthcare IT. Cloud strategies enable scalability, situational accessibility, disaster recovery, and other key benefits, while AI facilitates analytics and automation.
Brilworks, an acclaimed AWS consulting company, specializes in generative AI development and product engineering, allowing healthcare organizations to modernize legacy systems effectively. With plenty of experience in healthcare IT, we are geared towards offering customized solutions based on the needs of the healthcare organization while still being focused on interoperability, compliance, and patient outcomes.
Brilworks works with the popular cloud architecture to ease the transition of a healthcare organization with minimal disruption. If you are interested in starting your modernization process and seeing how Brilworks can support your journey, reach out to our team for a consultation.
Most projects take 6-18 months, depending on complexity and approach, with phased implementations offering quicker benefits.
Compare maintenance costs, productivity losses, and security risks against implementation costs and efficiency gains over 3-5 years.
No, hybrid approaches can balance legacy components with cloud capabilities while addressing security and compliance needs.
Use phased rollouts, thorough training, parallel systems, and schedule transitions during low-volume periods.
Prioritize HIPAA compliance, end-to-end encryption, robust access controls, and regular security assessments.
Get In Touch
Contact us for your software development requirements
Get In Touch
Contact us for your software development requirements